Carole Youakim, MD. Vice President of the LPS.
The LPS held its Summer Regional Meeting on August 31st and September 1st 2013 at La Maison de la forêt-Bkassine in South Lebanon. It was an opportunity to share knowledge and experience in a friendly setting. More than 50 delegates participated in this event.
[slideshow]
The meeting began on August 31st at 3pm by a presentation on Medical Registries and Health Care Awareness Campaigns done by Mrs Joumana Mansour.
Then, Dr Mirna Waked, President of the LPS, presented the results of the first epidemiological study done in Lebanon on Chronic Bronchitis and COPD and their correlates in Lebanese nonsmokers.
It was a cross-sectional study conducted between October 2009 and September 2010, using a multi-stage cluster sample all over Lebanon including Lebanese residents aged 40 and above with no exclusion criteria.
Smoking remains the strongest risk factor for COPD and chronic bronchitis but this does not preclude that both diseases can be found in non-smokers as well. Few studies among non-smokers have been conducted regarding the prevalence of chronic bronchitis and COPD and their predictors all over the world. This study showed that out of 2201 individuals, 732 were never-smokers: 25 (3.4%) of them had COPD, and 86 (11.75%) fulfilled the definition of chronic bronchitis. Correlates of COPD included a childhood respiratory disease, house heated by diesel, and older age. On the other hand, correlates of chronic bronchitis included childhood respiratory diseases, living in southern Lebanon versus other regions, heating home by gas, older age, number of smokers at work, and lower height.
Reference: Waked M, Salameh J, Khayat G, Salameh P. Correlates of COPD and chronic bronchitis in nonsmokers: data from a cross-sectional study. International Journal of COPD 2012: 7 577-585.
.
Thereafter, Dr Mireille Sfeir gave us an overview of the recent advances in pulmonary diseases in the years 2012-2013.
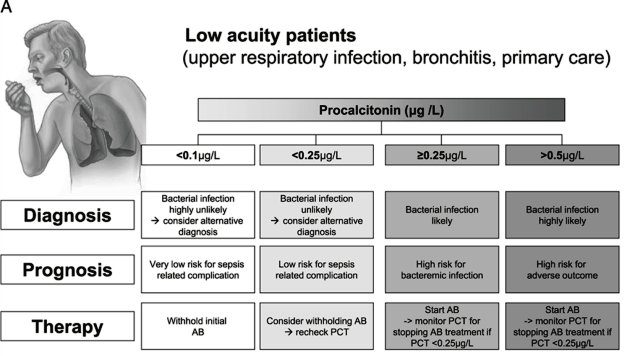
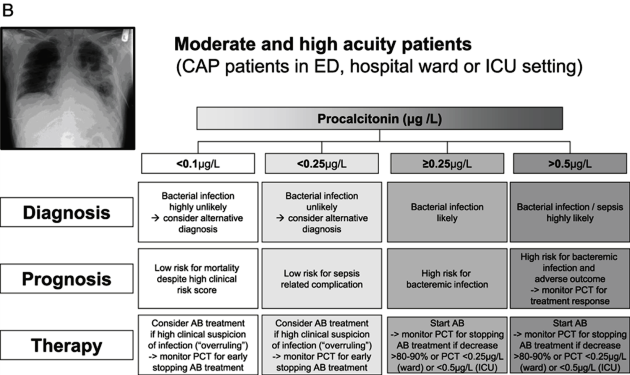
One of the topics covered was the role of procalcitonin in managing adult patients with respiratory tract infections. Although still relatively new on the clinical frontier, a series of randomized controlled trials have evaluated procalcitonin protocols for antibiotic-related decision making and have included patients from different clinical settings and with different severities of respiratory infection. In these trials, initial procalcitonin levels were effective in guiding decisions about the initiation of antibiotic therapy in lower-acuity patients, and subsequent measurements were effective for guiding duration of therapy in higher-acuity patients, without apparent harmful effects. Recent European respiratory infection guidelines now also recognize this concept.
Reference: Philipp Schuetz, Devendra N. Amin, Jeffrey L. Greenwald. Role of Procalcitonin in Managing Adult Patients with Respiratory Tract Infections. Chest 2012;141(4)1063-1073.
Another important subject was the role of B-type natriuretic peptide (BNP) guided algorithm for ventilation weaning. Difficult weaning from mechanical ventilation is often associated with fluid overload. BNP has been proposed as a tool for predicting and detecting weaning failure of cardiovascular origin.
In a randomized controlled multicenter study, patients were allocated to either a BNP-driven or physician-driven strategy of fluid management during ventilator weaning. In the BNP-driven group, furosemide and acetazolamide were given more often and in higher doses than in the control group. The BNP-driven strategy increased the number of ventilator-free days but did not change length of stay or mortality. The effect on weaning time was strongest in patients with left ventricular systolic dysfunction. The two strategies did not differ significantly regarding electrolyte imbalance, renal failure, or shock.
Reference: Dessap AM et all. Natriuretic Peptide-driven Fluid Management during Ventilator Weaning. A Randomized Controlled Trial. AJRCCM 2012;186(12)1202-1204.
The role of inflammatory biomarkers and exacerbations of COPD was also discussed. In a recent study published in JAMA, Thomsen M et all found that simultaneously elevated levels of CRP and fibrinogen and leukocyte count in individuals with COPD were associated with increased risk of having exacerbations, even in those with milder COPD and in those without previous exacerbations. Further investigation is needed to determine the clinical value of these biomarkers for risk stratification.
Reference: Thomsen M et all. Inflammatory Biomarkers and Exacerbations in Chronic Obstructive Pulmonary Disease. JAMA12; 2013;309(22):2353-2361.
An update on Pulmonary Fibrosis in Sarcoidosis was summarized. Up to 20% of patients with Sarcoidosis develop fibrotic lung disease. The development of pulmonary fibrosis is associated with significant morbidity and mortality. Complications of fibrotic pulmonary sarcoidosis include pulmonary hypertension and chronic aspergillus disease. Immunosuppression is not always indicated in end-stage sarcoidosis. Lung transplantation should be considered for patients with severe fibrotic pulmonary sarcoidosis, as mortality is high in these patients.
Reference: Patterson KC, Strek ME. Pulmonary Fibrosis in Sarcoidosis. Clinical Features and Outcomes. Annals of the American Thoracic Society 2013; Vol. 10(4) 362-370.
After we had our General Assembly at 5pm, we ended up this Afternoon by a Symposium on COPD presented by Dr Moussa Riachi. Take home messages for this Symposium were:
- Adjust FEV1/ VC to age
- Search well for undiagnosed cases of COPD
- Think to start treatment at an earlier stage
- ICS: stick to good indications and be aware of steroid resistance
- LABA subtypes are different with Indacaterol the strongest
- Tiotropium better than Salmeterol but as equal as Indacaterol
- Glycopyrronium as equal as Tiotropium (but faster effect)
- Combination Indacaterol/GLycopyrronium is a perfect combination (lung function and exacerbations)
- Combination ICS/LABA is equal to Tiotropium in exacerbations
- ICS/LABA subtypes are different
- Roflumilast reduces exacerbations especially in chronic bronchitis
On the second day, Dr Claude Ghorra gave us an outstanding presentation on the New Pathological/Molecular Classification for Pulmonary Adenocarcinoma.
Dr Ghorra emphasized that pathological diagnosis should be made according to the WHO classification and the International Association for the Study of Lung Cancer (IASLC) classification of adenocarcinoma:
- Specific subtyping of all NSCLCs is necessary for therapeutic decision-making and should be carried out wherever possible.
- Predictive immunohistochemistry should be used to reduce the NSCLC-NOS rate to fewer than 10% of cases diagnosed.
- Adequate tissue material for histological diagnosis and molecular testing should be obtained to allow individual treatment decisions.
- Re-biopsy at disease progression should be considered.
- EGFR mutation is a validated predictive marker for response and progression free survival with EGFR tyrosine kinase inhibitors in advanced lung adenocarcinoma.
- EGFR mutation status should be systematically analyzed—with sequencing as a standard—in advanced NSCLC with a non squamous histology
- ALK activity can be efficiently targeted by the TKI crizotinib, and routine testing for ALK rearrangements should be discussed where this drug is available.
- Detection of the translocation by FISH is standard, but immunohistochemistry may have a role in screening out negative cases.
Reference: International Association for the study of Lung Cancer/American Thoracic Society/European Respiratory Society. International Multidisciplinary Classification of Lung Cancer. Journal of Thoracic Oncology. Volume 6, Number 2, February 2011.
Then, Dr Ahmad Hosari gave us a Symposium on Xolair and discussed the case of one of his patients with very severe asthma treated by Xolair.
Finally, before going to lunch, Dr Mirna Waked concluded by a Symposium on COPD and summarized the Pathos study comparing the combination of Budesonide/Formoterol to Fluticasone/Salmeterol in preventing exacerbations in chronic obstructive pulmonary disease. The aim of this study was to analyse Swedish healthcare utilisation data and compare the effectiveness of BUD/FORM and FLU/SAL in reducing exacerbations in matched patients with COPD.
The exacerbation rate was 26.6% lower with BUD/FORM vs FLU/SAL. The number needed to treat with BUD/FORM vs FLU/SAL to prevent one exacerbation per patient-year was 3.4. BUD/FORM was more effective than FLU/SAL after 1 year, with increasing benefit following longer periods of drug exposure. BUD/FORM-treated patients needed 16% fewer Tiotropium prescriptions per year than FLU/SAL-treated patients. BUD/FORM-treated patients had 22% fewer SABA prescriptions per year than FLU/SAL recipients. Fewer patients switched from BUD/FORM to FLU/SAL than from FLU/SAL to BUD/FORM.